4 & 5 June 2012
Universitas Hospital
Summary
The previous two days I have been working at the Universitas
Hospital on the University of the Free State Campus. I have learned a great deal about dietetics
by visiting the wards, ICUs, working in the milk kitchen (where supplements are
made), and going to meetings with the dieticians and doctors. I have also observed some major differences
between American and South African hospitals.
Detailed Account
Over the past two days I have learned a variety of useful
knowledge in many aspects of the Universitas Hospital. First off I have learned a great deal about
dietetics and have gained a vast respect for those who are and those who are becoming
dieticians. Second, I have observed an
entirely different hospital system compared to the familiar hospitals I have
been associated with in the United States.
Occasionally people tell me that even if I don’t learn anything while I’m
here I will return home with a new found respect for what my country has to
offer, this is becoming true more and more.
A run-down of what I have done and learned…
1)
Early mornings seem to be unnecessary but it’s
what this week entails. I get picked up
at 7:15 only to sit on a bench until 8:45 while the dieticians have their
morning tea and I dose in and out of sleep.
Nonetheless by the time we are ready to start I have usually caught up
on my sleep deprivation.
Yesterday morning I worked with a
dietician, learning about her patient’s in the neurology ICU and the renal
clinic. There were 4 people in the
neurology unit each with their own surgeries and treatments. Many black people have aneurysms because 80%
of their population has high blood pressure, therefore causing an aneurysm and
possibly renal failure. Another patient
has resided in the neurological ICU for over 70 days due to a cancerous tumour
that was removed from his neck. His isolated
recovery has been slow and minimal.
Twice a week full blood assessments are
taken of the patients. The dieticians analyze
these, along with the height, weight, and age of the patient in order to
prescribe the correct type and amount of feedings. The most important aspects of the blood work
are…
·
White Cell Count is a marker of infection if too
high.
·
Red Blood Cell Count, Electrolyte &
Hemoglobin levels are indicators of amount of blood loss from surgery.
·
Albumin levels can indicate poor absorption in
levels are too low and is an indicator of the nutritional status.
The neurological patients are usually feed
via a feeding tube that runs from their stomach up through their esophagus and
emerges from their nose. If a feeding
tube is impossible to use for one reason or another supplements will be given
intravenously as TPN. Once the patient
is well enough they will begin to eat a puree diet, followed by a soft diet and
then a normal diet. During this time
they will usually be switched from ICU to a high care area and then to the
wards.
2)
We then proceeded to the renal clinic where
there was an L shaped row of about 20 people receiving hemodialysis. The dietician explained that when the kidneys
fail most people begin peritoneal dialysis (PD) before beginning
hemodialysis. PD is a dialysis treatment
that the patient does 4 times every day, beginning at 6 a.m. and ending at 10
p.m. During each round of PD fluid
enters the body through a permanent tube and then is drained via the force of
gravity. Patients involved with PD can still
work and go about a relatively normal lifestyle. They must remain clean and change the bag
four times daily (each change taking about 20 minutes) in a sterile
environment.
 |
| Peritoneal Dialysis Cycle |
The basics are the same for all types of
dialysis, to remove waste from the body since the kidneys are no longer
able. The downside of hemodialysis is
that it is a large time commitment and usually involves giving up a “normal
lifestyle.” Patients on hemodialysis
must come to the clinic every other day to receive 4 to 5 hours of dialysis for
the remainder of their lives, unless they are fortunate enough to have a kidney
transplant.
 |
| Basic Cycle of Hemodialysis |
When a chronic kidney disease is diagnosed
it is important for the patient to understand they must participate in a
lifestyle change as well. Because they
are unable to pass urine it is imperative that they do not over hydrate and
experience a fluid overload. If too much
fluid is present pulmonary edema could be a result causing more severe health
conditions. The dietician sits with a
new patient and assesses the foods that were currently being eaten and revises
their diet to better suit their needs.
The dietician can also prescribe supplements, some provide 1000 kJ of
energy and 9 g of protein in as little as ½ a cup of liquid.
3)
That afternoon I went to the milk kitchen to
learn and help out. This is where the
supplements are made for all of the residing patients. The dietician prescribes a different mixture
of food/supplements for each patient and changes the amount or type when they
see fit. These diet needs are then sent
to the milk kitchen where the two staff whip up all of the necessary food. First we weighed the powder supplement, and
then measured warm water. We mixed the
two together and sometimes added sweetener to make the supplement more
palatable. Once the mixture was complete
we poured them into specific bottles and labelled them. Once we completed that task we went about the
hospital delivering them to each ward and having nurses sign that the food and
supplements were received. They do this
each day because the supplements are most beneficial up to 12 hours after they
are made. The ladies that work here are
wonderful people who truly love their job but welcomed an extra set of
hands.
 |
| The lovely Milk Kitchen Ladies |
4) Now on to today…once again it was an early
morning. Along with a 4th
year student there is also a second year student working in the clinical
setting this week. The 4th
year student gets her own patients and is constantly doing assignments and
having to answer questions on the spot while the 2nd year student
and I stand by learning and asking questions if we don’t understand
something. The majority of my confusion
lies at the fact that I don’t understand Afrikaans.
Much like yesterday I began around the same
time and worked with a dietician in her wards.
We began in the theatre (surgery) ICU.
There were many interesting and vastly unique cases in this
department. Our first patient had a
cancerous tumour removed from their esophagus.
During surgery a nasogastric feeding tube was inserted into the jejunum
to ensure proper feeding. The tube was
not placed in the stomach because it is imperative that no food travel up the
gastroesophageal sphincter from any sort of reflex. If this tube were to come out it would be
impossible to reinsert without surgery so feeding would have to be switched to
intravenous feedings which is more costly.
Our second patient was one of the most impacting of the day. He was admitted on Friday, having been beaten
with a pipe. He immediately went to the theatre
for neurosurgery due to his head trauma.
He also suffers from 3rd degree burns over the entirety of
his face due to being dowsed with boiling water. Due to the high risk of infection and being
unstable feeding has still not been established. Another patient received a colectomy and
ileostomy. During the surgery the
patient suffered from an increased pressure and leading to compartment syndrome
so the doctors did not close her abdomen.
Her surgery finished by placing a sterile bag over the opening which may
close itself or they will return when appropriate to stich her up.
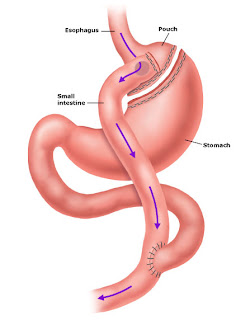
After visiting the patients we talked with
the dietician about Bariatric Surgery, similar to Gastric Bypass surgery in the
states. Tomorrow we will go to a
presentation on it and I will have more to report. As of now the process to be accepted for the procedure
is…Dietician -> Endocrinologist -> Dietician -> Physiotherapist (must
lose 5-10% of body weight) -> Psychiatrist -> Social Worker (if
necessary) -> Surgeon (for clinical evaluation) -> Surgeon (surgery)
-> Plastic Surgeon (skin removal, augmentations)
5)
I was then transferred back to the dietician I
was with the previous day and we went on ward round with some of the medical
students. This was extremely interesting
to me although I assume it was extremely overwhelming to the patients. There was a medical professor, 2 students in
residency, 3 students studying, the dietician, a dietetics student, and myself
all huddled inside of curtains surrounding a single patient. Even more traumatizing, in my opinion, was
the fact that some of the time the patient didn’t speak the language that we
were discussing them in, but I’ll get to that in the next section.
We did the rounds on the kidney disease
floor and the impacting cases were varied.
Our first patient was an obese woman, with known hypertension, who had
extreme edema due to Nephrotic Syndrome.
I have never seen that much swelling, it appeared as if she had been
stung (and allergic) to bees all over her body with the amount of
swelling. She could barely close her hands
or scratch an itch due to the edema encompassing her body. Another interesting patient was a 16 year old
boy, who looked, aside from lacking energy, looked perfectly normal and healthy
from the neck up and hips down. The
strange thing was his protruding abdomen that looked like the belly of a woman
who was 9 months pregnant. From his
thin, brittle, and copper like hair we could tell he had been malnourished
which could have caused Nephrotic Syndrome resulting in a large amount of fluid
in his Abdomen.
What I found to be most interesting during
this time was the amount of information we could determine by examining the
fingernails of patients. Half and half
fingernails refer to nails that appear to be divided in two, a whiter portion
by the cuticle and an upper pink portion.
The half and half nails are a common indication of renal failure. We
also examined the young boy’s fingernails which had faint white bands across
them, signalling a sign of Nephrotic Syndrome.
I am intrigued at how much information this small part of our body can
tell us.
 |
| Half & Half fingernails, indicating renal failure. |
 |
| White bands in fingernails, indicating Nephrotic Syndrome. |
6)
I once again went with the dietician from the
previous day as we assessed a new patient on PD. I was shocked to see that this man seemed
perfectly health at 26 years old yet because of his diagnosis of HTN in January
he would now be on dialysis for the rest of his life if he did not receive a kidney
transplant. He seemed very compliant and
not too down about the situation he was in.
He was smart and realized he would have to change his lifestyle if he
wanted to continue living and not enter complete renal failure. When a patient goes on dialysis the goal of
the diet is to be extremely low in salt and phosphorus. To do this the patient must not eat oranges,
grapes, peaches, coffee, chocolate, flavorings added to cool drinks (i.e. dark
drinks like coke and Pepsi), little amounts of milk, never any salt, alcohol or
chips. After interviewing the patient
about their current diet we explained to him what the foods he ate did to his
body and what foods he needed to substitute.
The patient currently lives off of a 1,200 rand (~$160 USD a month) pension
with his mother and sister, so it puts a perspective on how limited his funds
are for eating a nutritional diet.
7)
I then followed yet another dietician in and out
of a multitude of wards. We began at the
Ear, Nose, and Throat (ENT) Ward where the majority of the patients had a type
of pharynx or esophgeal cancer. Most of
the patients had part of their upper digestive system removed and during
recovery are unable to talk. But the
dietician was incredible with her patients making sure they were okay and
comfortable in every way possible. There
was also a person who attempted suicide by swallowing drain cleaner and
therefore burning his esophagus. The
adjacent hall housed children of all ages with breathing problems. About half of the children lived with a tracheotomy
for breathing purposes and their voices were only a whisper. Many of the children were long term residents
of the hospital and attended school there as well.
 |
| Tracheostomy, how many of the children were able to breath. |
We then travelled down to the pancreas, geriatric,
dermatology and internal medicine ward.
We saw people tinted many shades of yellow (due to various increased
levels of Bilirubin) suffering from pancreas cancer. Unfortunately for these patients the
prognosis was not good and the staff did their best to make the patients
comfortable in their remaining time.
They geriatric patients overall were suffering from dementia and Alzheimer’s,
remaining confused for the majority of the conversations. Many times these patients will not know what
or when they ate or even if they ate so it is vital that the nurses keep a
detailed record of all the foods given.
Lastly we discussed the Stevens - Johnson syndrome. This commonly occurs when women are treated
with ARVs when they are 6 months pregnant.
Some of the women have a reaction to the treatment and develops a
hypersensitivity complex to the skin, causing the skin on the outside and
inside of the body to literally peel off.
This is extremely painful to the patient and very bland, high protein supplements
are prescribed to ensure no burning occurs during digestion.
8)
Lastly we attended a meeting with doctors about
the patients suffering from diseases of the digestive system. Here we discussed the treatments taking place
for each individual patient and what the next steps are for treatment
options. Tomorrow we will visit the 7
patients we discussed in the meeting to understand the true extent of their
condition and prescribe/modify the appropriate diets.
A run-down of some of the
differences I’ve observed between US hospitals and the Universitas Hospital
a)
So as a
preface, I don’t know why I am shocked at what I’ve noticed and found at the
hospitals. I think when I was at MUCPP
last week I expected poor conditions because the clinic was in the middle of
the township. The hospital is much more
up to date than the clinic yet still far behind the standards in the US. I think I should not have expected as much
before going because I am in a third world country but I am just surprised by
many of the aspects that are daily occurrences here.
b)
The first thing I noticed was in the ICU rooms
there are multiple beds. The majority of
the time intensive care patients share a room with many other (~4) patients
that are also in severe recovery states.
After a few visits though this didn’t bother me as much.
c)
It is interesting that the floors can be so
incredibly different in the hospital. As
I walked up and down the stairs I always noticed one tiled floor that was
different, much cleaner and nicer than the others. When we stopped on this floor we first passed
through a guarded door. As the dietician
talked with the head nurse I glanced around and mentioned this is what a
hospital kind of resembles in America. I
was then told that this was the private floor of the hospital therefore only
people with Medical Aid (insurance) could be treated here. Instead of random free posters on the walls
there were pictures; overall the floor was much more respectable. It was if I had stepped into a different hospital
entirely as I entered the doors. I am
bit lacking of words for my opinion on this aspect (which may be a good thing
since I am supposed to be writing about my observations and not opinions).
d)
I am taken back with the lack of glove use. Over the past two days I haven’t seen any
nurse, doctor, or dietician (although I haven’t been in the operating rooms)
use gloves. I’m not sure if they have
gloves to use and choose not to wear them or if they do not have the funds to
wear gloves. It makes me feel very
wasteful that I use multiple pairs of gloves a day doing research when people
really need them for safety here. I was confounded
when I watched a nurse take the blood of a newly diagnosed HIV + patient
without gloves on. I am still quite
speechless on this subject.
e)
The hospital itself is much older and has much
less new aged equipment than most of the hospitals I have previously been
to. This was expected, but what was
unexpected was a hospital with 6 elevators but only 1 working
elevator. This elevator had to be used
to transport machines, food supplements, and most importantly unhealthy patients
to different floors of the 10 story hospital.
I am shocked that they do not have funds so repair the elevators in the
hospital and they have been broken for over a year now. I can only imagine what would occur in the
event of an emergency and hope that we never have to find out.
Due to the lack of elevators and the
constant stairs I take daily I assumed that people would be more fit in this
atmosphere. Much to my surprise I’m not
sure if I have ever seen more overweight and obese person in one building. I can easily say that 90% of the nursing
staff is overweight and the majority of the time I see a multitude of perfectly
capable people waiting for the elevator.
Every now and again you will see a patient trudging up the stairs
suffering from a respiratory condition.
On the other hand I have seen people force others out of the elevator in
order to get a patient in a wheelchair to another level. Surprisingly it isn’t only on the way up,
people will wait 10 minutes just to catch an elevator going down. I am discouraged to observe the lazy
lifestyles and obesity epidemic throughout the world.
f)
This is a short and simple observation. I am surprised to see that every doctor, dietician,
etc. keeps their cell phone on loud throughout the day. They will completely stop mid-sentence to
answer their phone even when they are with a patient. I’m not sure if this is the way the hospital
contacts them or what the etiquette is but I find it very strange and somewhat
disrespectful for the patients.
g)
This is one of my most astounding observations
to date, the language barrier. Before
traveling to South Africa I knew there were 11 official languages spoken. There are 3 main languages spoken where we
are residing, English, Afrikaans, and Sesotho.
I knew this would be a problem for me but I didn’t realize how much of a
problem it creates in the medical profession.
Often doctors are treating people who are
referred from the townships (locations) and the primary home language there is
Sesotho. Some people from the locations
also speak English while most of the doctors, being white, speak
Afrikaans. This creates a large problem
when asking the patient questions and communicating what is happening to the
patient. Many times throughout the day
we had to find a nurse that spoke a certain language so we could communicate
with a patient.
I found myself trying to imagine being in
some of the patient’s positions and I was completely terrified. Imagine you are sick and not quite sure what
is wrong with you. No family is by your
side when suddenly a green curtain is pulled around you bed (in a room of 4
people) for privacy. Nine people of skin
colors you may have never seen before surround your bed and begin to talk in a
language you do not understand. They
pick up your hands and poke and prod around your body before asking you “do you
speak Afrikaans or English.” You
continue to lie there confused until they repeat the question. Afrikaans,
English they are familiar words so you respond “Sesotho.” A nurse then appears who becomes a rough
translator between you and your surrounding barricade of people. After a few questions you are asked if you
have any question (which patients never did) and then the people that have your
fate in their hands are gone before you know it. To me this would be an incredibly
traumatizing experience but maybe that is because where I come from. This could be expected and perfectly normal
in my current environment.
h)
Lastly I found it odd that almost all of the
patients were alone, although they were in a room with up to 3 other
people. Very few had any family or
friends by their side supporting them. I
know in my family when anyone is in the hospital we all are by their side for
support and assistance. It was difficult
for me to surround the 16 year old boy I mentioned above in 5. He was alone, surrounded by 9 people and
spoken Sesotho. He was just a boy and
scared, his boy was turning against him and it appeared that he had no one. I wasn’t the only one who felt this way as we
left I saw two people squeeze his arm telling him it would be okay and giving
him a warm smile as the tears welled up in his eyes.
Logically thinking I know people must
continue to work if they have jobs and that is probably what pulls them away
from the hospitals. They must continue
to support the other family members they have and transportation to the
hospital can be extremely expensive.
Many of the people referred to the Universitas Hospital live 60 or more kilometres
away. I realize how unlikely it is for
families to visit, it was a difficult experience for me.
Over the last two days I have learned lots of information
and been astounded more than once.
Primarily I have learned to be much more grateful for what my country
and my family has to offer me. South
Africa is doing the best they can and they are on the right path but I
am thankful for many of the privileges America has to offer. I cannot begin to express my gratitude for my
family for having the ability and choosing to support me throughout my own life
and hardships.
This place is life changing.