6 June 2012
Universitas Hospital
Summary
Detailed Account
Since my blog was so long yesterday I was hoping for the
initial shock and learning from the hospital to be over but that was not the
case, so it looks like it’s going to be anther fairly long blog… I think I’ll divide it up again into the dietetics/education
learning (numbers) and then into the environmental/cultural observations
(letters).
1.
I began with rounds in the gastrointestinal, oncology,
etc. wards, once again a large group of doctors and dieticians. The most threating patient I saw during this
time was suffering from insulin dependent type 2 Diabetes. He was a non-compliant patient and recently
partook in alcoholic endeavours. His life
choices resulted in gastroparesis, a difficulty during gastric emptying. Therefore he must eat small low-fat meals
frequently although he could no longer stomach these in his severe
condition. The dietician switched up to
a diabetic supplemental fluid which he also vomits. The next obvious choice would be to feed him
with TPN intravenously but many doctors balk at this idea because having an IV
in for a long period of time increases the risk of sepsis. At this point the most important thing is
that the patient receives nourishment before starvation occurs. To repair his gastroparesis a jejunal
extension is required for the patient to go home with a permanent feeding
tube. Unfortunately the Universitas
Hospital’s extension expired in 2001 so they are at a loss for a plan of action
at the moment.
2.
I went about with many dieticians today but some
was repetitive of yesterday so I won’t go into that today. We were given an extremely interesting
presentation on Bariatric Surgery (aka Gastric Bypass). In order to qualify for the surgery in South
Africa one must have a BMI above 40 or above 35 along with comorbidities. The Universitas Hospital is only given a
small amount of money to perform such surgeries; therefore they can only take
about 10 patients per year. Due to their
low cost circumstances they usually only consider patients with a BMI of over
50. Comorbidities fall into many
categories including; metabolic, cardiovascular, respiratory, gastrointestinal,
urological, dermatological, neurological, endocrine, reproductive,
psychological, and musculoskeletal.
As of now
the process to be accepted for the procedure is…Dietician -> Endocrinologist
-> Dietician -> Physiotherapist -> Psychologist -> Social Worker
(if necessary) -> Surgeon (for clinical evaluation) -> Surgeon (surgery)
-> Plastic Surgeon. In this process
the dietician refers the patient to the appropriate doctors and follows the
patient for assessments throughout. The
endocrinologist evaluates the diseases that the patient has and varies the
dosage of the medications based on the weight and health of the patient. The physio teaches the patient exercises they
can do to help with mobilization and losing 5-10% of their body weight before
the surgery can be performed. The psychologist
assesses the compliance and dedication of the patient along with previous issues
like depression and eating disorders.
The surgeon/physician will determine if a patient is a good candidate
and ready for the operation. Lastly
usually after a year or most a plastic surgeon will help with skin removal and
augmentations.
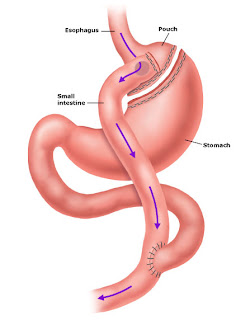
We mostly
focused on the sleeve resection surgery and the Roux-en-Y gastric bypass
option because those are the two offered at the hospital. The sleeve surgery closes off a portion of
the stomach, connecting the esophagus to the duodenum (first portion of the
small intestine). This appears to one
long tube, resembling a banana. During the
Roux-en-Y surgery a new stomach pouch (roughly the size of a quarter is created
and directly connected to the jejunum (middle portion of the small intestine).
 |
| Gastric Sleeve Resection |
 |
| Roux-en-Y Gastric Bypass |
2 Weeks
pre-op: low volume diet
Day 1
(post-op): NPO (Nothing per Orem, nothing through the mouth)
Day 2/3 –
4: Clear liquids in small sips waiting 10-15 min between sips
Day 5 - 14:
Full liquids up to 60 mL at a time in small slow sips (ex. Smoothie, soup, Ensure)
Day 14 - 28:
Pureed food up to 150-200 mL at a time in small slow sips (1 min between)
Day 28 - 42:
Soft foods blended or chewed very well, no fruit skins
6 Weeks:
gradual return to pre-op diet, 150-200 mL with vitamin, mineral, multivitamin,
Iron, B12, folate, and calcium supplements forever
It is important
that patients do not drink during meals or 30 minutes before or after a meal
because they have a high risk of experiencing feelings of ‘dumping syndrome.’ Since there is such little space in the
stomach the food and liquid must fight for the area, therefore the food could
be regurgitated or pass to quickly for nourishment.
We were
fortunate enough to meet a successful patient who had received a sleeve
restriction 7 months prior. He began at
232 kg (512 lbs) by the time he met the dietician and proved he was a candidate
for surgery he had reached 216 kg (476 lbs).
At this point in his life he was practically immobile, walking with a
cane and becoming short of breath rapidly.
He was morbidly obese on Glucophage for Diabetes and also suffered from
gout and joint pain. When he went in for
surgery he was at 205 kg (452 lbs), losing almost 10% of his body weight. Today he is still obese but he glows
throughout at 175 kg (386 lbs). He is
completely off his Glucophage and one of the friendliest and most optimistic
people I’ve met. I am positive he will
continue making wonderful progress throughout the next years and will maintain
his healthy weight.
a.
I found it incredibly unsettling some of the
inadequacies the hospital and patients have to face due to a lack of
funds. Previously I mentioned the tube
that had expired in 2001, to obtain that tube would take 6 months and by then
the patient would be dead. I was also
told today that a patient had been in tremendous amounts of pain after a
surgery but the hospital was out of morphine so they had to substitute with a
lesser pain medication. They are doing
the best they can with what they have but it is disappointing that this is all
one of the best hospitals has to work with.
b.
I must say the dieticians are wonderful at their
jobs. They are all extremely well educated
and know their material through and through.
They are also very caring and personable with their patients. Patients appear to brighten up a bit with the
dietician enters and they enjoy sharing and learning about how to live
healthier lives.
c.
I realized our ethical procedures are much more
strict in America than they are here or in the enforcement here. On many occasions I have noticed people
discussing a patient’s conditions and personal issued (even regarding HIV) in
the open and in other patient’s rooms. I
am a bit bewildered at the openness and lack of privacy/confidentiality but it
seems common.
d.
I have made a discovery…there are gloves lurking
about the hospital!!! Unfortunately they are not being used in the most optimal
ways. I observed a woman taking blood
today and she used a glove as the tourniquet, but not on her hands for her own
safety…interesting.
No comments:
Post a Comment